Are we looking in the right place for answers?
- Adam Rinde, ND
- Sep 19, 2025
- 6 min read
How the future of microbiome testing will be more precise.
A commentary on the study:
Tap J, Derrien M, Törnblom H, et al. Fecal and Mucosal Microbiota Profiling in Irritable Bowel Syndrome and Inflammatory Bowel Disease. Front Microbiol. 2019;10:1655. doi:10.3389/fmicb.2019.01655
I began studying stool and the gut microbiome in 2005–2006. Back then, Great Smokies Laboratory (later known as Genova Diagnostics) was one of the few labs offering stool testing to assess foundational microbiome imbalances, such as Lactobacillus and Bifidobacterium levels, along with screening for pathogens and pathobionts. These early tests paved the way for addressing dysbiosis through the use of probiotics, prebiotics, herbal therapies, and even conventional antimicrobials.
Since then, the field has evolved dramatically, from basic culture techniques to 16S rRNA sequencing, shotgun metagenomics, and now even AI-informed stool.
But we are still studying fecal samples – whereas the real knowledge may be in the microbiome sample from the mucosal lining.
Studying the fecal microbiome is akin to a detective examining the garbage bins outside a house to determine what happened inside. You’ll find clues; maybe some shredded documents, a broken dish, or a food wrapper- but you’re still one step removed from the actual scene of the crime.
In contrast, sampling the mucosal microbiome is like walking into the house itself. You see what is on the walls, the fingerprints on the doorknob, the scuff marks from a struggle. It’s messier, more complex to access, but far more revealing about what went down.
Suppose we are going to use the microbiome as a precise lever to help balance conditions like Inflammatory Bowel Disease (IBD) and Irritable Bowel Syndrome (IBS).
In that case, we need this precise data.
The tools currently available, although continually improving, are still predictors and signals rather than true diagnostic tools for the microbiome signature from a pathology perspective.
The study: Tap J, Derrien M, Törnblom H, et al. Fecal and Mucosal Microbiota Profiling in Irritable Bowel Syndrome and Inflammatory Bowel Disease. Front Microbiol. 2019;10:1655. doi:10.3389/fmicb.2019.01655 helped show the difference between fecal profiles of the microbiome vs. the mucosal sample of the microbiome in IBS, IBD, and Healthy Controls.
Here is a rundown on the structure of the study:
Study Objective
To characterize and compare the fecal and mucosal-associated microbiota composition in individuals with Irritable Bowel Syndrome (IBS), Inflammatory Bowel Disease (IBD: Crohn’s and ulcerative colitis), and healthy controls, to identify disease-specific microbial signatures and potential biomarkers.
Key Takeaway
Mucosal microbiota, more than fecal samples, provide disease-specific microbial signatures that help differentiate IBS from IBD, highlighting the critical diagnostic potential of mucosa-associated microbial profiling.
Design
Cross-sectional, observational, multicenter study using high-throughput 16S rRNA gene sequencing for microbiota profiling.
Participants
214 individuals:
IBD Group: 67 participants (36 Crohn's Disease, 31 Ulcerative Colitis)
IBS Group: 70 participants
Healthy Controls: 77 participants. Age range: adults, matched across groups. The gender distribution was balanced, although specific percentages are not provided. Inclusion criteria included diagnosis confirmed by clinical, endoscopic, and histologic criteria. Exclusion criteria included the use of antibiotics or probiotics within the past month and other gastrointestinal diseases.
Study Parameters Assessed
Microbiota composition (16S rRNA sequencing of fecal and colonic mucosal samples)
Alpha and beta diversity metrics
Inflammation status (histological data)
Disease subtype, location, and activity status
Primary Outcome
To identify distinct fecal and mucosal microbial signatures that differentiate IBS and IBD from each other and from healthy controls.

Key Findings
IBD mucosal microbiota were marked by decreased alpha diversity and increased Proteobacteria (notably Enterobacteriaceae), especially in inflamed tissues.
IBS samples showed intermediate dysbiosis with elevated Erysipelotrichi, Parabacteroides distasonis, and Prevotella copri and a microbial signature more similar to controls than IBD.
Fecal samples did not distinguish disease subtypes as well as mucosal samples.
A machine learning classifier based on mucosal taxa correctly predicted health vs disease status (AUC = 0.85), but struggled to differentiate IBS from healthy controls or IBD from IBS (AUC = 0.60–0.67).
IBD inflammation status correlated with distinct microbial patterns, notably enriched Proteobacteria and reduced butyrate producers (e.g., F. prausnitzii)
Transparency
The study was part of the IBIS cohort supported by European Union's 7th Framework Programme and the Swedish Research Council. Authors declared no competing financial interests.
Mechanisms
The study explored several key microbiome-related mechanisms:
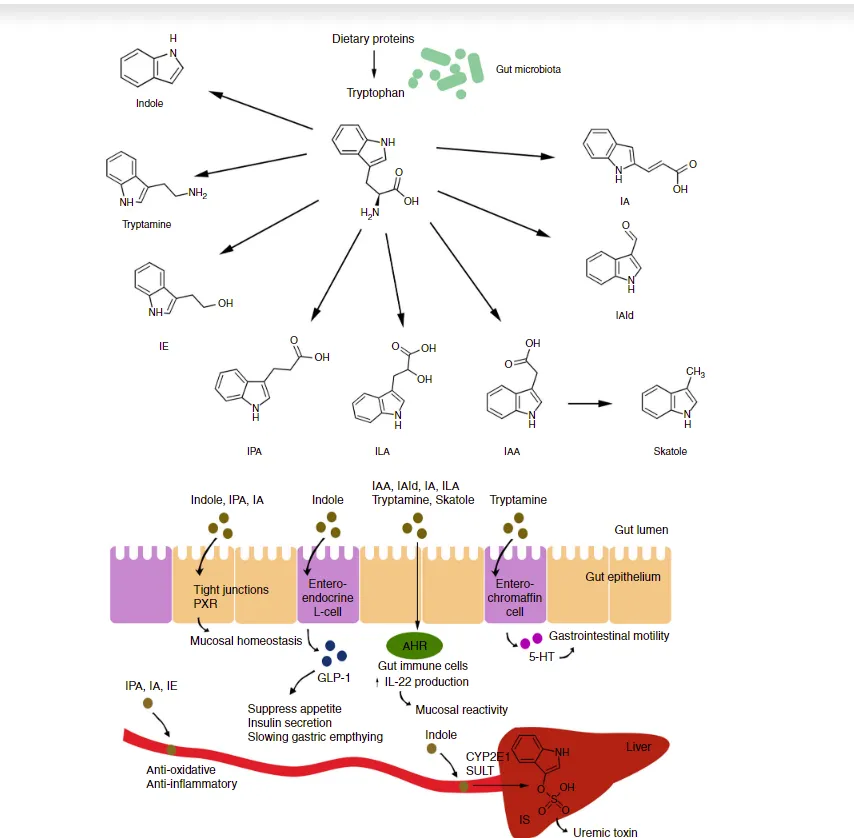
Dysbiosis-associated inflammation in IBD was linked to a loss of butyrate-producing bacteria and an overgrowth of Proteobacteria, consistent with epithelial barrier disruption and immune activation.
IBS-associated symptoms may be related to metabolic imbalances caused by Prevotella and Parabacteroides, which can affect bile acid metabolism and gas production, potentially influencing visceral hypersensitivity and motility.
The mucosal interface (rather than stool) may drive host-microbiota interactions and inflammation more directly.
Takeaways
This study included a well-characterized cohort and the dual sampling approach. However, the cross-sectional design limits interpretation of causality. It remains unclear whether microbial changes drive disease or reflect host responses.
Furthermore, while the study’s machine learning classifier performed well in distinguishing between health and disease, it struggled to differentiate IBS from IBD—a sobering reminder that microbiome diagnostics are not yet ready to fully replace clinical judgment or histopathology.
Mechanistically, the depletion of Faecalibacterium prausnitzii and Ruminococcaceae in IBD patients reinforces what we already know about the role of SCFAs and mucosal barrier integrity.
Similarly, the overrepresentation of Erysipelotrichi and Parabacteroides in IBS supports prior research linking these taxa to bile acid dysmetabolism and epithelial irritation, which are often clinically addressed through the use of bile binders, microbiome repair protocols, or elemental diets.
This study stands out for its direct comparison of stool and mucosal samples in IBS and IBD.
One of the perennial clinical challenges is distinguishing subclinical inflammation (as in IBS or early IBD) from overt immune activation.
Stool samples only tell part of the story.
This is why I have been a staunch advocate of running gut inflammation markers in parallel with stool microbiome testing (ie, fecal calprotectin, fecal lactoferrin, fecal Secretory IgA, Fecal Eosinophilic protein X). And even assessing for intestinal permeability markers, such as those in the Cyrex Array 2 panel. Equally important is evaluating short-chain fatty acids and analyzing bile acids.
The coupling of stool analysis with inflammation markers gives us the most actionable data.
While stool testing remains widely used due to its non-invasiveness, this research suggests that mucosal microbiota are more reflective of local immune activity and disease-specific pathophysiology.
It's likely that in the future, mucosal microbiome sampling will become a standard part of colonoscopy follow-up for IBD patients, especially as our understanding of host-microbe interactions deepens. For IBS patients, non-invasive technologies like smart capsules may eventually provide a practical way to sample the mucosal environment without the need for endoscopy.
In my clinical practice, I use the Proteobacteria dominance and Short Chain Fatty Acid production deficiency as a signature for dysbiosis intervention regardless of IBD or other disease conditions.
Point blank, this signature is a clue of loss of the oxygen gradient, inflammation upregulation, and the need for gut lining repair. In this environment, the commensal microbiome generally needs to be rebalanced. However, this study serves as a warning: Mucosal dysbiosis can occur in the absence of overt changes in fecal microbiota.
One thing that is an actionable thought to be used today….
The presence of Prevotella copri and Parabacteroides distasonis in excess in IBS patients suggests the need for caution with prebiotic therapy.
In patients who worsen on FODMAPs or fiber-rich regimens, these taxa may contribute to the reason why.
Another important insight from this study is the role of bile acids and their metabolites in gut health. When balanced, bile acids can have anti-inflammatory effects, but when dysregulated, they may contribute to an inflammatory gut environment. For certain patients, it may be clinically appropriate to explore bile acid binders in conjunction with strategies to support the growth of secondary bile acid–producing microbes, such as Clostridium scindens.
In any clinical situation, we want to be more like a Marine, getting down to the ground floor and surveying the situation with great detail. Yet, sometimes we only can be a land surveyor and look at bigger patterns, making predictions based on clinical presentation and available data.
If all disease begins in the gut, we are getting closer to the Marine view of disease.
===================================
If you want to be involved in an in-depth gut conversation with me join my Gastrointestinal Solutions Circle by going to: https://gastrointestinal-solutions.circle.so/checkout/membership-inaugural