Unpacking Tryptophans Role in Gut Health
- Adam Rinde, ND
- Aug 7, 2025
- 4 min read
Before I get into this post, I want to share that in this world of AI there is a larger belief that all answers can be extracted by chatting with a machine. Realize that those of us who write and have a practice are sharing our soul, inspiration, experiences, trials, and tribulations. Plus, we have skin in the game. This stuff matters to us. Mediocracy can be achieved with machines, but mastery of one's craft and a caring and loving human spirit is still left to us humans....enjoy the post.
----------------------
Much. research in gut health involves Tryptophan. The amino acid many Americans associate with Thanksgiving!
Specifically, the research involved Tryptophan’s role in the Kynurenine pathway and Indole pathway.
We are going to talk about the Indole Pathway.
This pathway is critical to understand for anyone with digestive issues. Especially for unsolved brain fog, bloating, and constipation, even on a low-FODMAP diet. Many years ago, a patient once asked me, “ I eat no carbs, so how can I be bloated?” I was stumped a bit until I learned about the indole pathway.
Now, don’t be taking a post-turkey nap on me! Do you get the reference?
This story begins with the amino acid tryptophan, which we consume in our diet and is sourced from protein. The top sources are meat, poultry, fish, eggs, dairy, nuts, and seeds.
When we consume protein, some of the tryptophan escapes digestion and reaches the colon, where specific microbes metabolize it. In cases of SIBO, this may happen in the upper intestine.
These tryptophan-metabolizing microbes include Clostridium, Escherichia coli, Lactobacillus, Peptostreptococcus, and potentially Ruminococcus species.
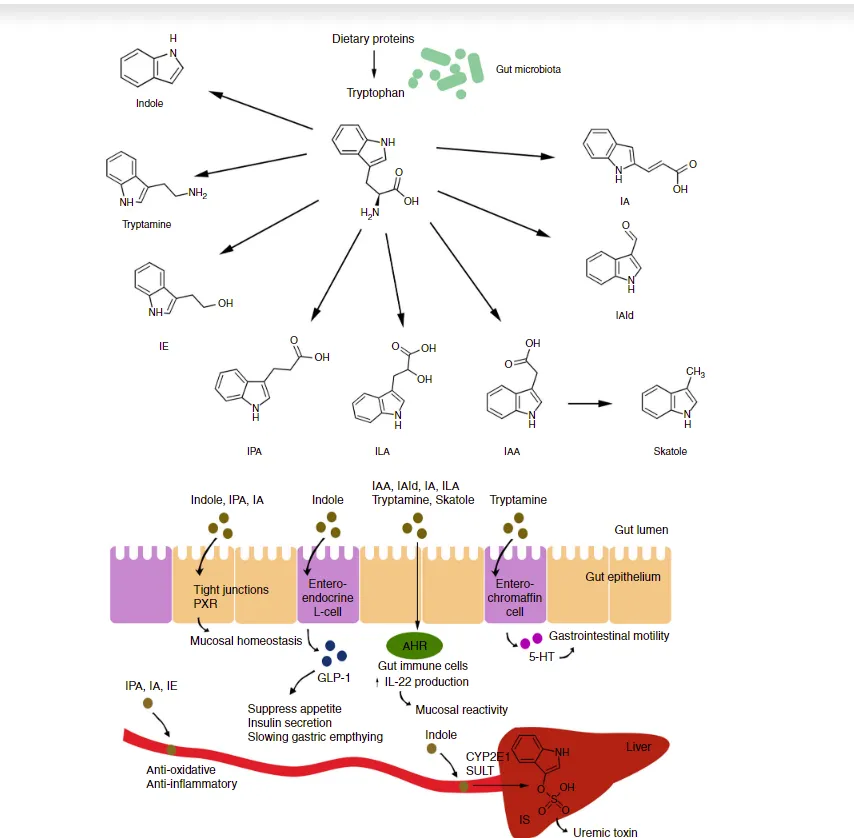
Their metabolic products can include beneficial compounds like indolepropionic acid (IPA) and Indole-3-aldehyde (IAld) and harmful ones like indole and skatole.As you can see, these compounds have multiple effects on gut function.
Tryptophan metabolites can be anti-inflammatory and protect gut junctions (IPA), as shown on the left of the picture. As shown, Indole, IPA, and IA activate PXR (Pregnane X Receptors), which is involved in sealing the gut and making it less leaky.
In addition, tryptophan metabolites such as IAld can protect the gut barrier by stimulating the mucus membrane and mobilizing the immune system by activating the AHR receptor (shown in green).
In particular, Lactobacillus species (e.g., L. reuteri, L. johnsonii, L. acidophilus) use tryptophan to produce IAld. This helps protect the gut lining, supports immune balance, and may prevent dysbiosis-related inflammation.
Now the downside.
Indole-producing microbes play a key role in tryptophan metabolism within the gut microbiota. The most well-known producer is Escherichia coli, which expresses the enzyme tryptophanase (tnaA) to convert tryptophan into indole, pyruvate, and ammonia. Other common indole-producing bacteria include species of Bacteroides, Clostridium, Proteus, Klebsiella, Enterobacter, and Peptostreptococcus.
These microbes contribute to the intestinal pool of indole and its derivatives, some of which have beneficial effects, such as modulating intestinal barrier function via activating the pregnane X receptor (PXR).
Excessive indole production or dysregulated metabolism; particularly into indoxyl sulfate ; can lead to inflammatory and toxic effects, especially in individuals with impaired gut-liver-kidney axis function, such as those with chronic kidney disease.
While indole levels, in moderation, can support gut health, their conversion to indoxyl sulfate creates a uremic toxin that promotes oxidative stress and vascular inflammation.
Connected but slightly different is Ammonia production.
Ammonia production in uremia does not arise from indole metabolism but from a separate microbial process involving bacterial urease activity. When urea accumulate; due to kidney dysfunction or high-protein diet; and encounters urease-producing bacteria such as Proteus and Klebsiella in the gut, it is broken down into ammonia and carbon dioxide. This ammonia can increase gut pH, disrupt the intestinal mucosal barrier, and contribute to symptoms such as bloating, inflammation, and brain fog, particularly in individuals with compromised gut-liver-kidney axis function.
So the ammonia story can be a separate but parallel process with Indole pathway issues.
Indole has a related compound called skatole (3-methylindole), which is also derived from tryptophan via microbial metabolism. When produced in excess, skatole is associated with gut inflammation, halitosis, and foul-smelling stools.
Skatole-producing microbes include Clostridium spp. (particularly C. scatologenes and C. putrefaciens), Bacteroides, Peptostreptococcus, Fusobacterium, and Porphyromonas spp. These microbes may become problematic when overgrown or overfed with dietary tryptophan, especially in dysbiosis and poor gut barrier integrity
.So what to do?
Know your microbiome. The only way is to test it regularly. To balance your microbiome, work with prebiotics and microbial herbs.
Test for metabolite production. Metabolomix testing through a Diagnostic Health Solutions lab that can show you your plasma/urine levels of some of these metabolites
Realize that too much or too little tryptophan may be a problem. The general rule of thumb is to consume 0.8 grams to 1 gram of protein per day for each Kg of body weight. Strive for balance.
Ensure proper digestion of tryptophan. Too much or too little stomach acid and poor digestion of proteins may be over-delivering or under-delivering tryptophan to the gut.
Tryptophan is good.
Too little is not beneficial, and too much is not helpful.
Explore your balance and improve it.
The gut will likely be less bloated, less inflamed, and less reactive.
Your mind will likely be clearer.



