Overtraining Immune issues buffered by probiotics
- Adam Rinde, ND
- Apr 29, 2025
- 3 min read

Immunosuppression due to overtraining is a big deal in endurance athletes.
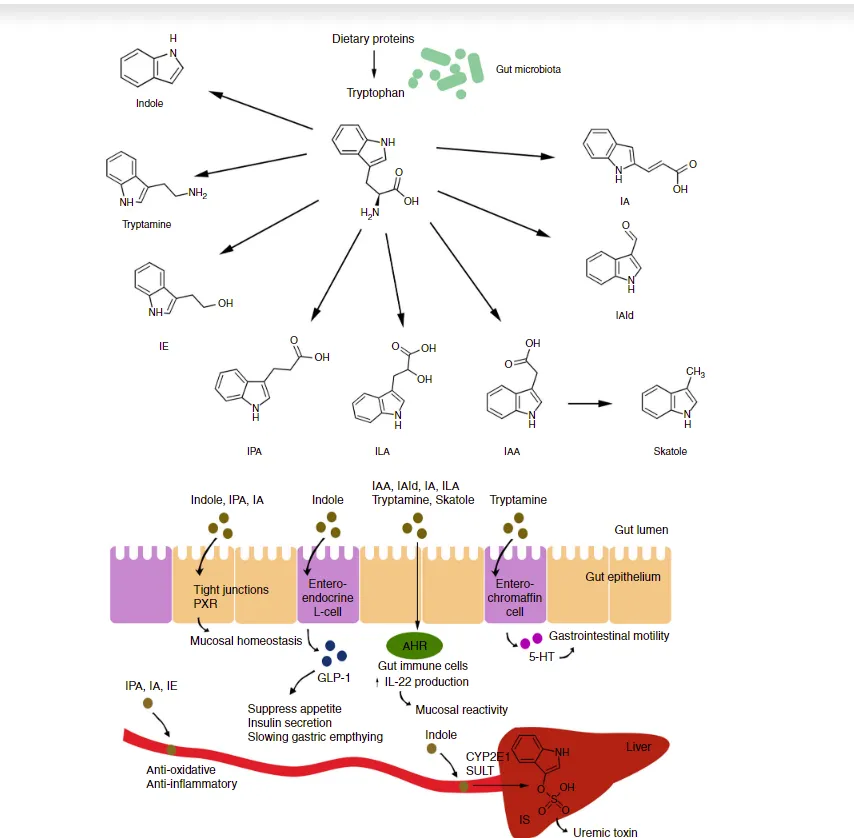
The thinking is that the overtraining might activate Indoleamine 2,3-dioxygenase (IDO-1).
When IDO-1 is overactive, it uses up tryptophan and can push a pathway leading to immunosuppression.
Thus, overtraining may reduce host immune defense, potentially increasing susceptibility to common upper respiratory tract viral infections.
. This is thought to occur partly because IDO-1 activity supports the induction and function of regulatory T cells (Tregs), promoting an immune-tolerant environment.
Being immune-tolerant is good except when you have an infection.
Meaning, T-reg activation is significant if your body is trying to stop a harmful immune system activation strategy (like autoimmunity ), but not so great if your body is trying to fight off a virus.
Bring in the regulatory T cell (Treg). Regulatory T cells have a protective role in infection by limiting pathogen-induced immunopathology, while allowing the development of immunological memory. However, they can be a key strategy for pathogens to induce survivability.
Suppressing the activation of regulatory T cells or their cytokine production is a promising approach for developing therapies for chronic infections and cancer.
Yet, it risks promoting inflammation and autoimmunity.
Recently, I read the paper: Probiotic Supplements Beneficially Affect Tryptophan–Kynurenine Metabolism and Reduce the Incidence of Upper Respiratory Tract Infections in Trained Athletes: A Randomized, Double-Blinded, Placebo-Controlled Trial" by Barbara Strasser and colleagues, published in Nutrients in 2016.
In this nicely designed study, probiotic supplementation in training athletes cut down on Upper Respiratory infections (URTI) in a double-blinded placebo-controlled study (N=33)
Subjects were given 1 × 10^10 colony-forming units (CFU) of a multi-species probiotic (Bifidobacterium bifidum W23, Bifidobacterium lactis W51, Enterococcus faecium W54, Lactobacillus acidophilus W22, Lactobacillus brevis W63, and Lactococcus lactis W58) or placebo once per day for 12 weeks. The findings:
URTI incidence: 79% of the placebo group vs. 35% of the probiotic group experienced URTI symptoms (p = 0.016).
Tryptophan levels: Post-exercise Trp decreased by 11% in the placebo group (p = 0.02) but remained stable in the probiotic group.
Kyn/Trp ratio: Increased in both groups post-exercise, but more favorably modulated in the probiotic group.
Training adherence: Probiotic users had significantly higher weekly training volumes (8.0 vs. 6.6 hours/week; p < 0.001).
Before supplementation, 10 subjects on placebo and 12 on probiotics experienced one or more upper respiratory tract infections over the prior three months. After 12 weeks of treatment, 11 subjects on placebo and 5 subjects on probiotics experienced one or more Upper respiratory symptoms during the study period
They measured serum concentrations of tryptophan, phenylalanine, and their primary catabolites, kynurenine and tyrosine. They also determined the concentration of the immune activation marker neopterin at baseline and after 12 weeks, both at rest and immediately after exercise.
Why this matters: Prolonged or intense physical training can induce a transient immunosuppressive state. The kynurenine pathway, activated via IDO-1 during inflammation or immune stress, depletes tryptophan, a critical amino acid for serotonin and NAD+ synthesis. Tryptophan depletion is associated with lowered immune competence, increased infection susceptibility, and central fatigue.


Consider probiotic support for athletes, especially during winter or periods of overtraining.
Microbiome modulation could be an adjunct strategy in patients with ME/CFS, post-viral syndromes, or autoimmunity in which IDO-1 activation is implicated.