Could my stomach acid be too low?
- Adam Rinde, ND
- Jun 12, 2025
- 6 min read
Updated: Jun 24, 2025
Recently, a patient came in complaining of bloating and belching after meals. Additionally, they experienced an uncomfortable feeling of fullness and early satiety. There was also slight discomfort or indigestion after meals.
In medicalese, this is a classic diagnostic puzzle.
This patient had gone down the rabbit hole of tests, including an endoscopy that ruled out Helicobacter pylori and gastric cancer. Nothing was found.
When in doubt, what do gastroenterologists do? Try a proton pump inhibitor and a prayer to see if it works.
This is not only a safe bet, but it also feeds the $3.3 billion proton pump inhibitor empire. If the proton pump inhibitor works, the problem is solved, according to the Gastroenterologist.
But, wait? “Am I supposed to take this for the rest of my life?” …exactly. That is another story and another problem. It asks, “What are the long-term implications of being on proton pump inhibitors?”.
Also, what if taking a proton pump inhibitor makes symptoms worse?
Well, in that case, we may be looking at a condition called hypochlorhydria (low stomach acid).
Hypochlorhydria, a condition characterized by low stomach acid production, can have a wide range of impacts on digestive health. Let's explore the causes, consequences, and potential treatments for this condition.
First, let’s talk about how stomach acid made:
Stomach acid is made in the parietal cells of the stomach. In coordination with the hormone gastrin, acetylcholine stimulated by the vagus nerve, and histamine, the stomach’s parietal cells will release stomach acid.


Causes of Hypochlorhydria
Several factors can contribute to hypochlorhydria, ranging from infections to neurological, autoimmune, and age-related changes:
H. pylori Infection:
Helicobacter pylori is a known cause of hypochlorhydria. It produces urease, an enzyme that neutralizes stomach acid, disrupting the gastric lining. Over time, this can lead to gastritis and atrophic gastritis, reducing the function of acid-secreting parietal cells. (see Saha, et. al. 2010)
Vagus Nerve Issues:
The vagus nerve stimulates stomach acid production by activating parietal cells through acetylcholine. Dysfunction caused by traumatic brain injury (TBI), neurodegenerative conditions, dysautonomia, or chronic stress can impair this signaling, leading to reduced acid production. (see , The Power Of Exhale)
Aging:
Stomach acid production naturally declines with age. With aging, there is an increased prevalence of atrophy of gastric cells. Atrophy leads to age-related alterations in the gastric mucosa, which include a reduction in the number of parietal cells responsible for acid production. Sometimes this is referred to as atrophic gastritis. (See Choi, et.al. 2016)
Dysautonomia:
The autonomic nervous system is crucial in regulating gastric functions, primarily through the vagus nerve, which stimulates gastric acid secretion and motility. Dysautonomia can lead to impaired vagal tone, resulting in decreased gastric acid secretion. Reduced parasympathetic output, a hallmark of this condition, leads to impaired stimulation of parietal cells and decreased acid production. (See McMenamin, et.al. 2016)
Autoimmunity:
Autoimmune destruction of parietal cells, often associated with pernicious anemia, reduces hydrochloric acid and intrinsic factor production. This leads to impaired vitamin B12 absorption and contributes to hypochlorhydria.
Medications:
Several medications can interfere with stomach acid production, including:
Proton Pump Inhibitors (PPIs): e.g., omeprazole, pantoprazole.
H2 Blockers: e.g., ranitidine, famotidine.
Anticholinergic Drugs: e.g., atropine, scopolamine.
NSAIDs: These medications can cause gastritis, damaging the gastric lining and indirectly leading to hypochlorhydria.
Consequences of Hypochlorhydria
The consequences of hypochlorhydria extend beyond simple indigestion. Low stomach acid can have cascading effects on various digestive processes:
Impaired Digestion: Hypochlorhydria leads to protein maldigestion, as stomach acid is essential for breaking down proteins.
Disrupted Enzyme and Bile Release: Low stomach acid reduces the release of pancreatic enzymes and bile. These substances are crucial for breaking down carbohydrates, proteins, and fats in the small intestine. Reduced enzyme and bile release significantly impairs digestion and nutrient absorption.
Gastrointestinal Discomfort: Hypochlorhydria often manifests as digestive discomforts, such as belching, gas, and a feeling of fullness immediately after meals. These symptoms arise from the impaired breakdown of food in the stomach and altered motility.
Increased Risk of SIBO: Hypochlorhydria increases the risk of small intestinal bacterial overgrowth (SIBO) by creating an environment where bacteria can flourish, survive the stomach, and enter the upper intestine. Recently, I learned colonizing bacteria from our oral microbiome are often transferred via the 1-2 Liters of saliva we swallow daily. Stomach acid would typically sterilize this before it gets into the small intestine. SIBO disrupts digestion, interferes with nutrient absorption, and causes inflammation in the small intestine.
Immune System Activation: Undigested proteins, a consequence of low stomach acid, can trigger immune responses in the small intestine, potentially leading to food sensitivities and inflammation. This is what is thought to occur in intestinal permeability, also known as leaky gut.
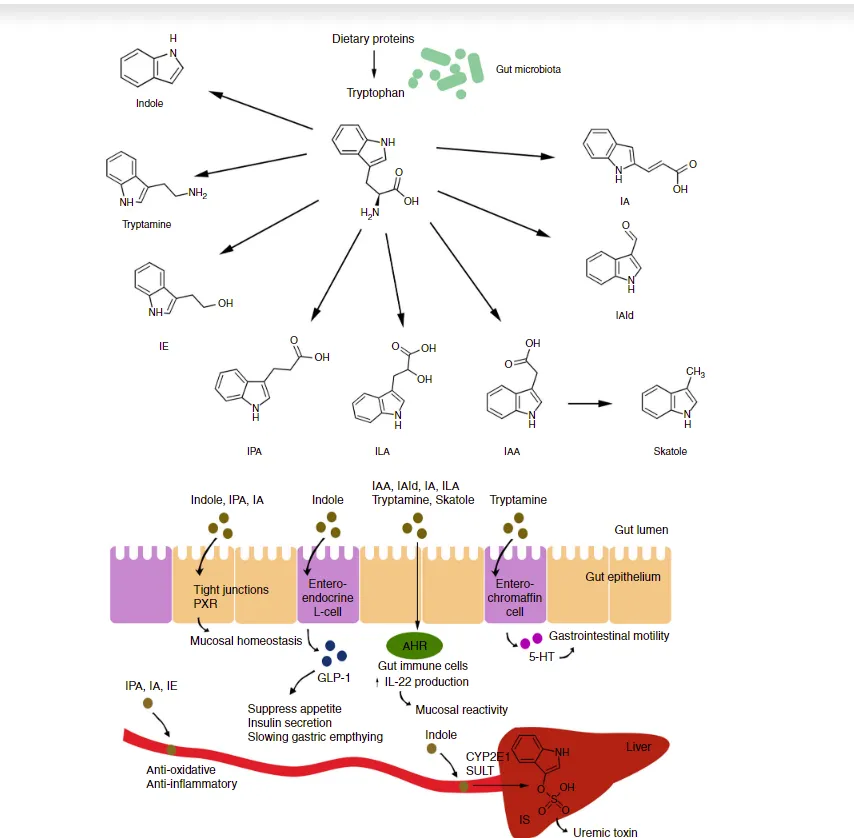
Gut Microbiome Imbalance: Stomach acid influences the composition of the gut microbiome. Hypochlorhydria can disrupt the balance of bacteria in the gut, potentially impacting overall health.
Clinical Manifestations and Implications of Hydrochloric Acid Deficiency
A deficiency in hydrochloric acid (HCl) can manifest clinically through various signs and symptoms, and it has implications for several bodily functions and overall health. HCl’s primary role is in digestion, but it also plays a crucial role in nutrient absorption and preventing pathogen overgrowth.
Symptoms:
Gastrointestinal symptoms are the most common indicators of low gastric acidity and can include:
Bloating after eating
Diarrhea or constipation
Flatulence
Heartburn
Indigestion
Food allergies
Nausea or nausea after taking supplements
Other signs include:
Hair loss in women
Low tolerance for dentures
Malaise
Soreness, burning, and dryness of the mouth
Weak, peeling, and cracked fingernails
Clinical Conditions:
Low gastric acidity has been associated with an array of clinical conditions, including:
Anemia
Arthritis
Asthma
Celiac disease
Chronic autoimmune disorders
Chronic candidiasis
Diabetes mellitus
Eczema
Osteoporosis
Various skin diseases
Nutrient Absorption:
HCl facilitates the absorption of numerous nutrients. Without sufficient HCl, the absorption of the following nutrients may be impaired:
Folic acid
Ascorbic acid (vitamin C)
Beta-carotene
Non-heme iron
Calcium
Magnesium
Zinc
B-complex vitamins
Pathogen Overgrowth:
The acidic environment created by HCl in the stomach acts as a defense mechanism, killing ingested pathogens and preventing the overgrowth of bacteria and fungi in the small intestine.
When HCl secretion is impaired, there is an increased risk of infections due to the survival of ingested bacteria. This can lead to:
Small intestinal bacterial overgrowth (SIBO)
Candida overgrowth, particularly in women using H2-receptor antagonists
Age-Related Decline:
Research indicates that HCl secretion declines with age. This decline in stomach acidity can harm nutrient absorption and increase the risk of various health problems in older adults.
How to know if I have low stomach acid?
Spoiler alert. Very few validated or practical solutions exist to test for hydrochloric acid deficiency. Mostly, diagnosis is made by symptoms and therapeutic correction, resulting in benefit.
Quasi-diagnostic tests, such as the Heidelberg pH capsule, exist to confirm low stomach acid. However, the validity of this test has not been confirmed.
In research settings and in some clinical settings, a swallowed wireless smart pill may be used to measure pH.
Treatment Options
Before starting treatment, it is recommended that you be evaluated for the root causes of low stomach acid and the consequences of low stomach acid as mentioned above.
It is very important to know beforehand if there is a H. pylori infection, autoimmune disease, or B12 deficiency. Also, any treatment would be contraindicated if a patient has gastric or duodenal ulcers.
Treatment often involves HCl supplementation, typically in the form betaine HCl or glutamic acid HCl.
In addition, apple cider vinegar and digestive bitters have been used.
Before starting treatment, we sometimes do the Apple Cider Vinegar Challenge.
The Apple Cider Vinegar Challenge involves consuming two tablespoons of apple cider vinegar to assess stomach acid levels. If no burning sensation occurs, it suggests low stomach acid, and HCL supplementation may be considered. However, if burning occurs, it could indicate gut inflammation that needs to be addressed first. PLEASE DISCUSS WITH YOUR HEALTH CARE PROVIDER BEFORE TRYING THIS.
I also recommend addressing the intestinal lining before considering HCL supplementation or apple cider vinegar. Herbal demulcents (i.e., mastic gum, DGL) and key nutrients such as zinc carnosine can be essential in restoring intestinal lining health.
Addressing the Root Cause: Treating the underlying cause of hypochlorhydria is vital for long-term management. This involves addressing issues like H. pylori infection, vagus nerve problems, or medication side effects.
As always, Dietary Hygiene should be addressed.
Hypochlorhydria is a complex condition with far-reaching consequences for digestive health. It is often overlooked and not discussed, but it must be part of any conversation about gut health issues.
Are you interested in a deeper dive into Gut Health with me? If so, become a patient or join my Gastrointestinal Health Solutions Community. Paid members of my Substack will receive a free six-month membership to the community.