Stress and its impact on Intestinal Epithelial Cells
- Adam Rinde, ND
- Jun 25, 2020
- 6 min read
Updated: May 2, 2021
Review of Gates of Wrath: Role of intestinal epithelial cells in Stress response Talk by Dr Jacob Allen, Nationwide Children’s Hospital Microbiome summit Brain/ Gut AxiS The brain and gut are intrinsically linked . The nervous system has been explored as being the link specifically the via the vagus nerve. Yet, more information is being revealed about how neurotransmitters and stress hormones may interface with the gut microbiome and effect gut function such as intestinal barrier function.
The vagus nerve (also known as cranial nerve X) is a bi-directional nerve that starts in the medulla of the brain stem and then spreads to various organs throughout the body including the lungs, the digestive tract and the heart. 80-90% of the vagus nerve is made of afferent sensory nerves which send feedback from the organ to the brain for an appropriate response.
A perfect example is the baroreceptors in the aortic arch artery which gain sensory feedback of flow going through the aortic arch and can send feedback to the brain to help adjust blood pressure.
Here is a functional break down of the vagus nerve.

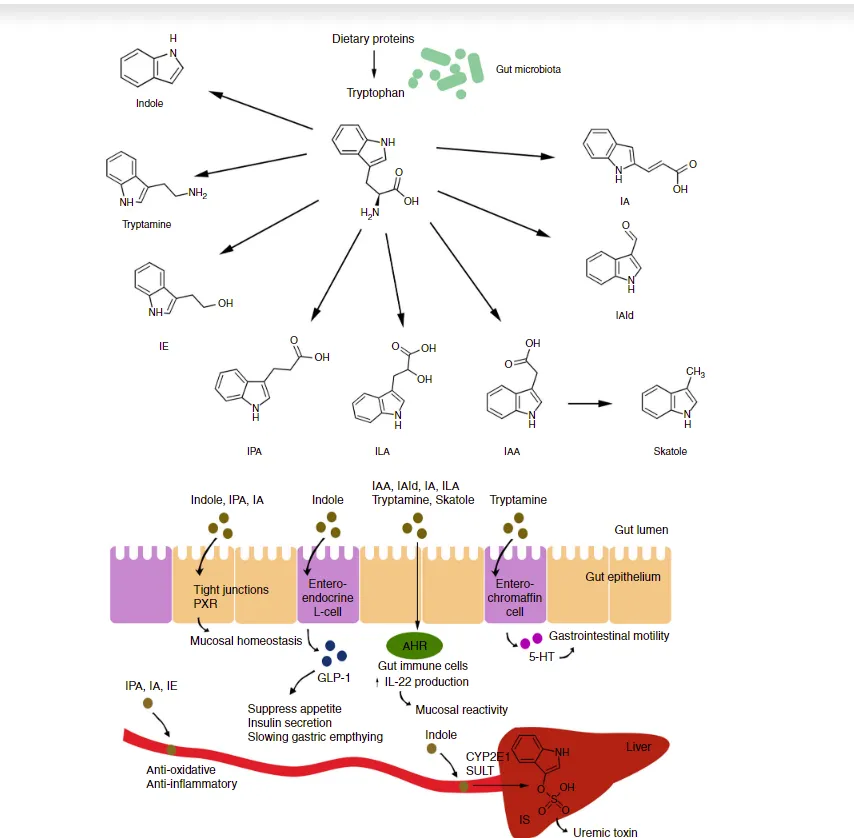
We can see that digestion , motility, and immune response is deeply influenced by ventral vagal nerve function. And lack of ventral vagal tone can lead to sympathetic overdrive and release of stress response that may act unfavorably on the gut. Research has shown specific species of microbiota are involved with production of neurotransmitters such as GABA, Norepinephrine, and Serotonin both directly and indirectly. And that pain, anxiety , and depression can cause alterations in the gut microbiota via release of catecholamines like noradrenaline.

In turn noradrenaline can cause certain microbes to survive and others to die-off. It can also potentially cause pathogens to emerge leading to inner intestinal mucosal layer breaches and and therefore intestinal permeability (see below) .

Based on Dionne et al., 2018; Struti et al., 2016; Moloney et al., 2016 and Montil-Castro et al., 2013 [22-25].
When the intestinal lining is breached then this because an immune event with cytokines are released that can further influence pain ,anxiety, and depression . Enteroendocrine cells can influence the release of serotonin as well. Interestingly , anxiety is a predisposing risk factor for post infectious IBS .
So this brings me to the talk I attended by Dr. Jacob Allen as part of the May, 2020 Microbiome Summit entitled Gates of Wrath: Role of intestinal epithelial cells in Stress response.
In the talk Dr. Allen mentioned that adding norepinephrine to a pathogen like E.coli results in growth and increase of shiga like toxin (he stated this was related to quorum sensing). And he also mentioned that high altitude training and military training has shown to alter the gut microbiota. This highlighted a core question of his research as to what would happen to the immune and mucosal defense of the gut barrier in rodents put under social stress and how this stress alters the gut microbiota.
Dr. Allen has pointed out that 11 out 14 studies showed positive relationship between stress and Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Disease (IBD), (Mawsdley and Rampton Gut (2005) . And that stress is a trigger for relapses in IBD (Jaghult, Gastroenterol Res. 2013). So, obviously this topic of brain/gut axis is highly critical in understanding how to manage and perhaps prevent IBS and IBD.
In Dr. Allen's' research they exposed mice to an environment called repeated social defeat. Basically they were living with an aggressor mouse for the experiences. They see this environment cause high sympathetic and HPA axis activity in the socially defeated mice.
In previous research by Dr. Amy Mackos ' stress did some predictable things including:
Increase Citrobacter rodentium infection
Increase inflammatory markers TNF-alpha and Nitric oxide synthase (inos0) were higher in stressed animals
Creates massive inflammation.
This was thought to be mediated by the common inflammatory pathway NF kappa Beta
Dr. Makcos and Dr. Allen's group published research in Frontiers Of Immunology to repeat the experiment in mice who couldn't make NF Kappa Beta. So these mice would be free of this inflammatory response (By the way turmeric reduces NF Kappa Beta).
And when the the mice lacked NF Kappa Beta they:
had reduced citrobacter infection
decreased epithelial inflammation
So that left him with a key question. Does stress lead to increased epithelial inflammation?
They did further study with social disruption studies. Genes associated with inflammation were highly associated with stress. 182 genes were altered by stress including Reg3B and Fut2. These are are two genetic pathways highly involved in the intestinal barrier.
The intestinal epithelial cells that were altered by cells had:
Increased TLR/NLR signaling (that is an immune response)
Increased Hypoxia (low oxygen)
Increased purine metabolism
Increased Glycoprotein biosynthesis
Glycoprotein biosynthesis is involved when the mucus layer is being disrupted and increased turnover. This is a key marker of intestinal permeability.
They then showed by imaging that the mucus layer in the stressed mice the mucus disruption was higher and the mucus thickness was thinner.
So the next question they had was if bacteria was getting through the mucus layer? So they measured LPS as a marker and stress in the mice raised LPS which is a marker of leaky gut. They wondered if the microbes driving the response in the intestinal epithelial cells? So they used Germ Free mice and the stressed the mouse in a similar experiment. And low and behold the inflammatory markers did not go up in germ-free mice. So they see that the link is highly related to the microbes. But the question still remained about how much the stress hormones played a role in the IEC response? In germ-free mice they stimulated mice with common drivers of intestinal inflammation specifically flagellin and lipopolysaccharide (LPS) and saw DUOX2 go up. Duox2(Dual Oxidase 2) is a protein found in the gut on the tip of the epithelium and is responsible for production of reactive oxidative species (ie. free radicals ) via hydrogen peroxide production. Interestingly and surprisingly, increased epinephrine, NE, cortisol added did not seem to play a role in inflammation. Hmm... Hard to say this is conclusive but that was his finding. He pointed out something that was considered a critical finding in his work ; DUOX2 went up in stress response. If DUOX is chronic stimulated it causes chronic inflammation and pathobiont growth. It has been showed DUOX2 is upregulated in CD and UC. Next they wondered if Duox2 elevation changed the microbiome.? They repeated the stress model experiment and looking at microbes that grew in stress and those that were downregulated . Upregulated was S24-7 , Enterohabdus, and Marvinbryantia and down regulated was Candidatus Arthromitus, Lachnoppiracea spp (obligate anaerobes). S24-7 (Candidatus Homeothermaceae) is highly upregulated in stress . It was highly related with DUOX2 and DUOXa2 expression. Why? Higher oxygen environment grows facultative anaerobes which have high catalase can break down catalase of hydrogen peroxide. They can survive a highly oxidative environment where others can not. He summarized that this creates a high oxygen environment which favors the growth of Facultative anaerobes grow bacteria that have the ability to break down Catalase . Obligate anaerobes usually don't break down Catalase. They concluded that S24-7 has high catalase activity.Another conclusion is that stress increases catalase activity.
Researchers are looking at these conclusions in humans. They have found that when studying stress in the microbiome in Crohn's Diseases. That low perceived stress vs. high perceived stress IBD patients had different microbiomes
A 2020 study that Dr. Allen participated in (Mackner, et. al .2020 . Psychoneuroendocrinology) showed that pediatric crohn's patients with high perceived stress grew parabacteroides which is a bacteria that has high catalase activity. Sme species of Parabacteroides may increase inflammation
So stress lead to increased survival of of certain potential pathogens.
My opinion. Treating IBD and IBS without addressing stress is missing a core component of treatment. Vagal nerve stimulation , lifestyle changes, counseling and herbal and nutritional treatments to help with anxiety and stress need to be a cornerstone of the IBD and IBS patient
I would advise any one who is concerned about the dysregulation of the HPA axis to first take my screening questionnaire here. And then consider the Adrenal Test that is offered by Precision Analytical Called the Dutch Adrenal . We can also look at Neurotransmitter Levels with ZRT Labs.
For more information send me a message.